The first CRISPR baby is turning 7. Scientists still can’t agree if she’s a miracle or a mistake. In 2018, Chinese scientist He Jiankui shocked the world by announcing the birth of the first gene-edited twins.
Six years later, the debate rages: Is CRISPR a tool for eradicating disease or a Pandora’s box of ethical nightmares?
What if we could eliminate genetic diseases forever? Sounds wonderful, until you consider the cost. This same technology that might free families from hereditary conditions could create “designer babies” only the wealthy can afford.
As CRISPR moves from labs to human embryos, scientists warn we lack proper safeguards. The question looms: can we harness this breakthrough without creating a genetic caste system?

Understanding CRISPR: The Science of Genetic Editing
CRISPR technology has revolutionized genetic research by making DNA modifications simpler and more accurate than ever before.
CRISPR-Cas9: “Genetic Scissors” Simplified
At its core, CRISPR-Cas9 functions as microscopic scissors for DNA, allowing scientists to cut genetic material at exact locations.
This system originally evolved in bacteria as a defense against viruses but now serves as a powerful tool in laboratories worldwide.
Scientists can target specific DNA sequences, make precise cuts, and then let cells repair the break—either by disabling a gene or adding new genetic material.
The process works through two main components: a guide RNA that locates the target DNA sequence and the Cas9 enzyme that cuts it.
Think of it like using Find and Replace in a document—the guide RNA finds the “typo” in the genetic code, and Cas9 cuts it out so corrections can be made. This precision makes CRISPR vastly more efficient than previous gene-editing methods.
What makes CRISPR truly revolutionary is its accessibility. The technology is relatively inexpensive and straightforward to use compared to earlier techniques, which has accelerated genetic research across fields from medicine to agriculture.
Germline vs. Somatic Editing: What’s the Difference?
Germline editing involves changing DNA in reproductive cells or embryos, creating modifications that will pass to future generations.
When scientists edit an embryo’s genes, every child and grandchild will inherit those changes—effectively altering the human genetic lineage forever.
This approach could theoretically eliminate inherited diseases from family lines but raises profound ethical questions about consent from future generations and unintended consequences that might not appear for decades.
Somatic editing takes a more conservative approach by modifying only non-reproductive cells in a living person.
These changes affect only the treated individual and cannot be inherited by their children. Scientists are currently using somatic editing in clinical trials for conditions like sickle cell anemia, beta-thalassemia, and certain cancers.
For example, doctors can remove blood cells from a patient with sickle cell disease, correct the genetic mutation, and return the healthy cells to the patient.
The distinction matters tremendously for regulation. Most countries permit somatic editing under careful oversight since it resembles traditional medical treatment, whereas germline editing faces strict restrictions or outright bans in many nations due to its far-reaching implications.
Beyond Cas9: Safer Alternatives Emerge

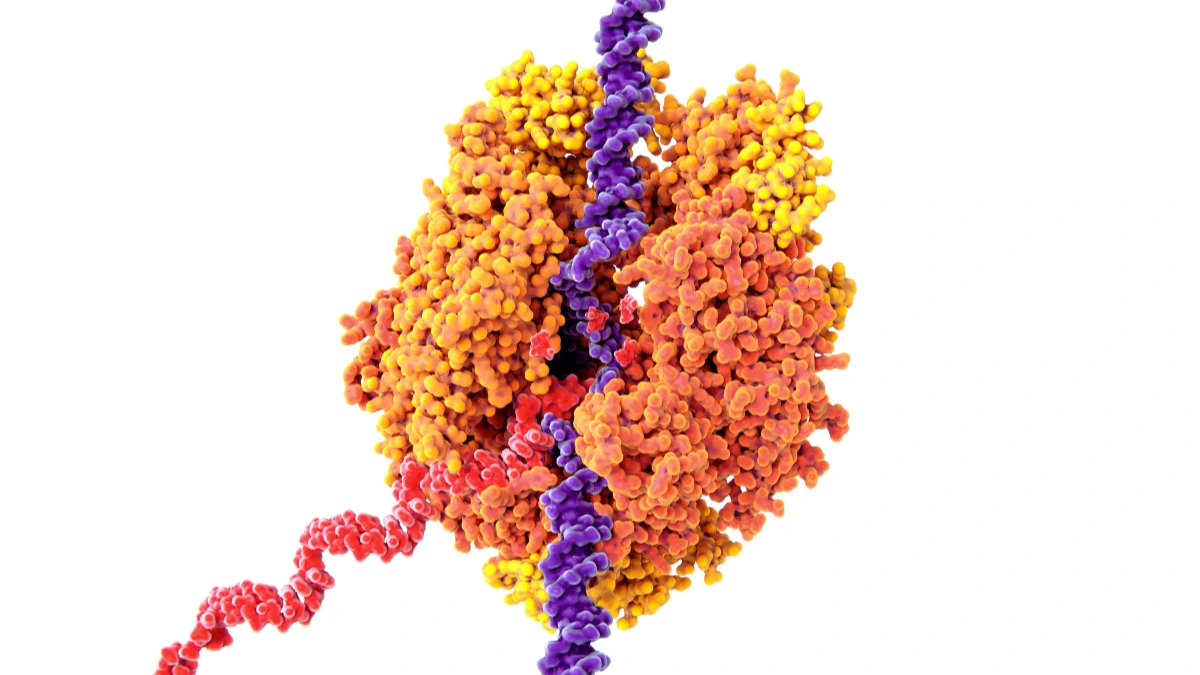
Base editing represents a significant advancement in precision genetic modification. Developed by Beam Therapeutics, this technique can change individual DNA letters without cutting both strands of the DNA helix.
Traditional CRISPR-Cas9 creates breaks in DNA that cells must repair, sometimes introducing unintended changes.
Base editing avoids this risk by chemically converting one DNA letter directly into another—like changing a C to a T or an A to a G—without breaking the DNA backbone.
Scientists have expanded the CRISPR toolkit with CRISPR-Cas13, which targets RNA rather than DNA. RNA carries instructions from DNA but degrades quickly in cells, making RNA editing inherently temporary and reversible.
This approach offers a safety advantage for treating conditions like macular degeneration or certain neurological disorders where permanent genetic changes might be risky.
RNA editing allows physicians to adjust treatment over time or stop if problems arise.
Both technologies address key concerns about conventional CRISPR. They reduce “off-target effects” (unintended edits at similar DNA sequences) and provide more control over the editing process.
As these tools mature, they may offer safer pathways to treat genetic conditions while minimizing risks associated with permanent DNA modifications.
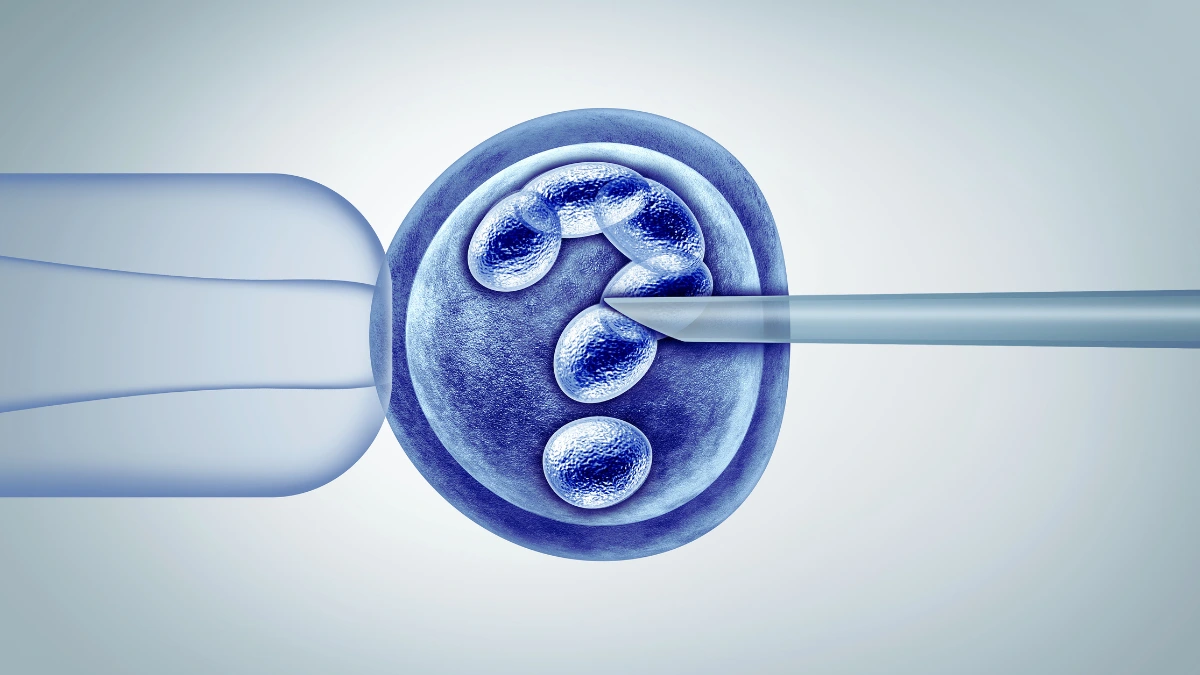
The He Jiankui Experiment: A Case Study in Hubris

In November 2018, Chinese scientist He Jiankui shocked the world by announcing he had created the first genetically edited babies.
His experiment targeted the CCR5 gene, aiming to make twin girls resistant to HIV infection—a goal motivated by their father’s HIV-positive status.
The scientific community immediately questioned both his methods and motives, pointing out that established techniques like sperm washing could have prevented HIV transmission without permanently altering the children’s DNA.
What especially alarmed experts was evidence of mosaicism in the edited embryos, meaning the genetic changes weren’t uniform throughout all cells.
This patchwork of edited and unedited cells left the children with unpredictable health outcomes and potentially new vulnerabilities.
Following international outcry, Chinese authorities investigated and ultimately sentenced He to three years in prison for violating medical regulations.
The case exposed serious gaps in oversight systems and prompted research institutions worldwide to strengthen ethical safeguards around gene editing research.
Scientists continue to monitor developments, concerned that this premature leap to human applications has damaged public trust in CRISPR technology’s legitimate medical potential.
Ethical Dilemmas: Cure Disease or Create Inequality?
The power to rewrite human DNA brings questions that science alone cannot answer, forcing society to weigh medical breakthroughs against social consequences.
Medical Necessity vs. “Designer Babies”

Most people support using genetic technology to eliminate devastating hereditary conditions.
Families carrying genes for Tay-Sachs, Huntington’s disease, or cystic fibrosis could have children free from these conditions, sparing future generations immense suffering. These applications represent clear medical necessities with broad ethical support.
However, the same tools that could eradicate disease could potentially enhance traits like intelligence, athletic ability, or physical appearance.
A Pew Research study reveals 71% of Americans oppose gene-edited babies, largely because of concerns about crossing this boundary.
The technology might start with preventing illness but could evolve toward creating children with genetic advantages based on parental preferences.
Such capability would transform reproduction into consumer selection, where genetic traits become commodities. Parents with financial means could select advantages for their children that others cannot access.
This raises profound questions about human dignity, equity, and whether genetic modification might stratify humanity into biological classes determined at conception rather than through life opportunities.
The Slippery Slope to Eugenics
History teaches caution about genetic manipulation. Early 20th century eugenics movements led to forced sterilizations and contributed to horrific human rights abuses.
Modern genetic technology operates in a different context but raises similar concerns about valuing certain genetic traits over others.
Without strict boundaries, genetic modification could create new forms of discrimination. Insurance companies might charge higher premiums to those with “unmodified” genes.
Employers could favor applicants with enhanced genetic profiles. Social pressure might force parents to modify their children to remain competitive.
As bioethicist Dr. Alta Charo from the University of Wisconsin warns, “Once enhancements begin, the line between therapy and privilege blurs irreversibly.”
The gatekeeping role would fall primarily to wealth. Only affluent families could afford extensive genetic screening and modification, potentially creating a genetic upper class with biological advantages from birth.
This scenario threatens to widen existing social gaps and create new hierarchies based on genetic capital rather than social opportunity, undermining democratic ideals of equal human worth.
Global Regulation: A Patchwork of Policies
Nations have responded to gene editing technology with vastly different regulatory approaches, creating inconsistencies that could allow controversial research to migrate to less restrictive jurisdictions.
WHO’s Guidelines and the Push for Transparency

The World Health Organization established its human genome editing registry in 2019 to track research globally and promote accountability.
This database aims to bring transparency to a field where secrecy had previously allowed rogue scientists to operate without oversight.
Researchers must register their experiments, methodologies, and results, creating a public record of all human gene editing research.
Meanwhile, the International Coalition of Medicines Regulatory Authorities (ICMRA) works to harmonize guidelines across borders.
Their framework emphasizes rigorous pre-clinical testing, ethical review boards with diverse membership, and long-term monitoring of subjects. These organizations push for consistent standards that balance scientific progress with ethical boundaries.
Despite these efforts, the registry lacks enforcement mechanisms. Participation remains voluntary, and no international body has authority to penalize violations.
Scientists conducting controversial research can simply avoid registration or relocate to countries with minimal oversight. This regulatory gap threatens to undermine global governance efforts as technology advances faster than policy.
National Approaches: From Bans to Loopholes

Countries have developed widely varying approaches to regulating CRISPR technology:
- United States: Federal funding cannot support research that creates or destroys human embryos. However, privately funded laboratories can conduct embryo editing research provided the embryos are never implanted. The FDA maintains authority over any clinical applications.
- United Kingdom: Operates through the Human Fertilisation and Embryology Authority, permitting embryo research under strict licensing for up to 14 days of development. Germline editing for reproduction remains prohibited.
- Canada: Takes one of the strictest approaches globally, with the Assisted Human Reproduction Act criminalizing germline editing with penalties up to $500,000 CAD and potential imprisonment.
- China: Following the He Jiankui scandal, implemented new regulations requiring national approval for clinical gene editing. However, oversight relies heavily on institutional ethics committees rather than centralized regulation.
- Japan: Recently relaxed restrictions to allow limited embryo research while maintaining prohibition on reproductive applications.
CRISPR’s Future: Miracle or Mistake?
The technology stands at a crossroads with potential to transform medicine and agriculture while simultaneously raising profound questions about its long-term impacts on society.
Breakthroughs on the Horizon

Clinical trials using CRISPR technology against sickle cell disease show remarkable promise.
Patients receiving genetically modified stem cells have experienced dramatic symptom reduction, with some becoming virtually disease-free after treatment.
This success offers hope for treating other blood disorders like beta-thalassemia and hemophilia that have long resisted conventional therapies.
Cancer treatment represents another frontier. Researchers are engineering immune cells to better recognize and attack tumors, with early trials showing encouraging results against certain leukemias and lymphomas.
Meanwhile, scientists at University of Pennsylvania are testing CRISPR-modified cells to target solid tumors, potentially expanding treatment options for previously untreatable cancers.
Agricultural applications may prove equally transformative. Scientists have developed gene drives capable of spreading specific genetic modifications through mosquito populations, potentially eliminating their ability to transmit malaria.
Similar approaches could address agricultural pests without chemicals, reduce Lyme disease transmission by ticks, or help coral reefs adapt to warming oceans.
Such ecological applications could save millions of lives but require careful testing to avoid unintended consequences in delicate ecosystems.
Risks of a CRISPR Divide
Market analysts project the global CRISPR industry will reach $37.2 billion by 2030, attracting massive investment from pharmaceutical companies and venture capital.
This commercialization drives innovation but also shapes research priorities toward profitable applications rather than public health needs.
Treatments for rare genetic disorders affecting small populations may receive less attention than cosmetic applications with larger markets.
Access barriers loom large as treatments emerge. The first approved CRISPR therapy for sickle cell disease costs over $2 million per patient, placing it out of reach for most people with the condition globally.
Health insurance in wealthy countries might cover such expenses, but patients in low and middle-income nations, where conditions like sickle cell are often most prevalent, face exclusion from these breakthrough treatments.
This creates a scenario where genetic medicine could actually widen health disparities rather than reduce them.
Wealthy populations gain access to genetic treatments while disadvantaged communities remain burdened by preventable genetic conditions.
Without deliberate policy intervention, CRISPR technology risks becoming another factor in global health inequality, contradicting the ethical principle that medical advances should benefit humanity broadly, not just privileged segments of society.
Call to Action: Safeguarding Humanity’s Genetic Future
The decisions made today about governing CRISPR will shape human biology and society for generations to come.
Demand Global Moratoriums

- Leading scientists and ethicists advocate for temporary but firm pauses on germline editing applications until fundamental questions can be resolved.
- Any moratorium should distinguish between somatic applications (which affect only individual patients) and germline modifications (which affect future generations).
- International scientific bodies like the National Academies of Sciences and Medicine recommend continuing basic research under strict oversight while prohibiting clinical applications of germline editing.
- Effective moratoriums require mechanisms for monitoring compliance and consequences for violations that cross international boundaries.
- Scientific journals can support these efforts by refusing to publish research conducted outside ethical guidelines, removing incentives for rushing applications.
Empower Public Oversight
- Genetic modification decisions cannot remain exclusively in the hands of scientists, corporations, or regulators without broader public input.
- Community engagement should include people from diverse socioeconomic backgrounds, cultural perspectives, and disability communities whose voices have traditionally been excluded.
- Patient advocacy groups representing those with genetic conditions must have meaningful roles in developing policies about editing those conditions.
- Educational initiatives can help citizens understand both the science and ethical dimensions of gene editing technologies.
- Deliberative democracy approaches like citizen assemblies offer models for incorporating public values into technical policy decisions.
Invest in Safer Alternatives
- RNA-editing technologies like CRISPR-Cas13 offer temporary modifications without permanent alterations to the genome.
- Base editing techniques that change single DNA letters without cutting both strands reduce risks of unintended chromosomal changes.
- Ex vivo approaches (editing cells outside the body before reintroduction) provide better control and verification than in vivo methods.
- Non-genetic interventions including prenatal screening, preimplantation genetic diagnosis, and conventional therapies may achieve similar goals with established safety profiles.
- Public funding should prioritize approaches that maximize medical benefits while minimizing irreversible changes to the human genome.
